Anti-SARS-CoV-2 receptor-binding domain
The receptor-binding domain (RBD) of the spike protein of SARS-CoV-2 is a critical component for viral entry into host cells, as it binds to the ACE2 receptor on human cells. Developing an anti-SARS-CoV-2 RBD could involve various strategies aimed at inhibiting this interaction, thus preventing viral entry and infection.
Antibodies:
Monoclonal antibodies: Monoclonal antibodies are laboratory-produced molecules that mimic the immune system's ability to fight off harmful pathogens such as viruses. Several monoclonal antibodies have been developed specifically targeting the RBD of the SARS-CoV-2 spike protein. These antibodies can bind to the RBD, preventing the virus from attaching to the ACE2 receptor on human cells and thereby neutralizing the virus.
Cocktail therapies: Some treatments involve using a combination of monoclonal antibodies targeting different epitopes on the RBD to reduce the risk of viral escape mutants that might arise due to single antibody therapy.
Passive antibody therapy: Monoclonal antibodies targeting the RBD have been used for passive immunization in individuals with mild to moderate COVID-19 to reduce the severity of illness and prevent progression to severe disease.
Vaccines:
mRNA vaccines: mRNA vaccines, such as those developed by Pfizer-BioNTech and Moderna, contain genetic instructions for producing the spike protein, including the RBD. When the vaccine is administered, cells in the body use these instructions to produce spike protein fragments, eliciting an immune response that includes the production of antibodies against the RBD.
Viral vector vaccines: Vaccines like the Johnson & Johnson's Janssen COVID-19 vaccine use adenovirus vectors to deliver the genetic material encoding the spike protein, including the RBD, into host cells, triggering an immune response.
Protein subunit vaccines: Some vaccines use purified protein subunits derived from the spike protein, including the RBD, to induce an immune response.
Peptide-based inhibitors:
Peptides derived from the RBD sequence or designed to mimic its structure can interfere with the interaction between the RBD and the ACE2 receptor. These peptides can be developed as potential therapeutic agents to block viral entry into host cells.
Small molecule inhibitors:
Small molecules are chemical compounds that can bind to specific sites on proteins, including the RBD, inhibiting their function. Small molecule inhibitors of the RBD-ACE2 interaction are being investigated as potential therapeutics against COVID-19.
Alternative Therapeutic Agents:
Nanobodies: Nanobodies are single-domain antibodies derived from camelid species. They offer advantages such as small size, high stability, and ease of production. Nanobodies targeting the RBD have shown promise as potential therapeutics against COVID-19.
Aptamers: Aptamers are short single-stranded DNA or RNA molecules that can bind to specific targets with high affinity. Aptamers targeting the RBD have been developed and evaluated for their ability to block viral entry.
These approaches represent diverse strategies for targeting the RBD of the SARS-CoV-2 spike protein, with the aim of developing effective therapeutics and vaccines against COVID-19. Continued research and development in this area are essential to combat the ongoing pandemic and prepare for future outbreaks.

Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection produces B-cell responses that continue to evolve for at least a year. Meanwhile, memory B cells are expressing increasingly large and potent antibodies that are resistant to the mutations found in the variants of concern1. Accordingly, vaccination of individuals recovering from coronavirus disease 2019 (COVID-19) with currently available mRNA vaccines produces high levels of plasma neutralizing activity against all variants tested1,2.
Here, we examine the evolution of memory B cells five months after vaccination with the mRNA vaccine Moderna (mRNA-1273) or Pfizer-BioNTech (BNT162b2) in a cohort of SARS-CoV-2 naïve individuals. Between priming and boosting, memory B cells produce antibodies that develop increased neutralizing activity, but there is no further increase in potency or extent thereafter. Instead, memory B cells that emerge five months after vaccination of naïve individuals express antibodies similar to those that dominate the initial response.
While individual memory antibodies selected over time by natural infection have greater potency and magnitude than antibodies elicited by vaccination, the overall neutralizing potency of plasma is greater after vaccination. These results suggest that boosting vaccinated individuals with currently available mRNA vaccines will increase plasma neutralizing activity but may not produce antibodies of an equivalent magnitude to those obtained by vaccinating convalescent individuals.
Between January 21 and July 20, 2021, we recruited 32 volunteers with no history of SARS-CoV-2 infection receiving either Moderna (mRNA-1273; n=8) or Pfizer-BioNTech (BNT162b2; n=24) mRNA vaccine for sequential blood donation. Paired samples were obtained at two or three time points. Individuals listed as "prime" were sampled an average of 2.5 weeks after receiving their first dose of vaccine.
Individuals who completed their vaccination regimen were sampled an average of 1.3 months after the booster (median = 35.5 days), which is not statistically different from sampling at 1.3 months in our cohort naturally infected3 (median = 38.5 days, P = 0.21). Individuals sampled at 1.3 months were sampled again approximately 5 months after the second dose of vaccine. The volunteers were aged 23-78 years (median = 34.5 years), 53% were male and 47% were female (for details, see Methods and Supplementary Tables 1 and 2).
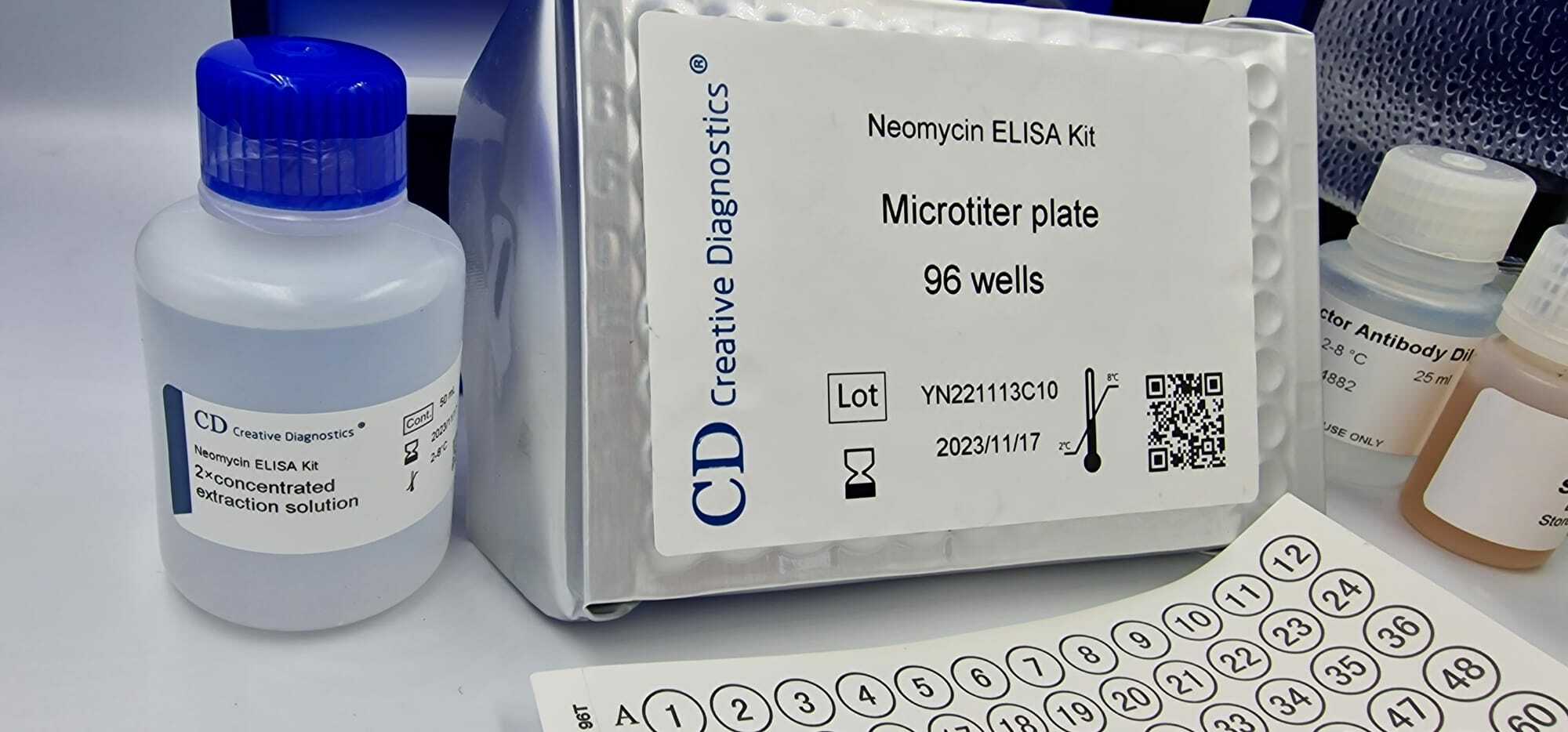
Plasma IgM, IgG and IgA responses to the receptor binding domain (RBD) of SARS-CoV-2 were measured by enzyme immunoassay (ELISA)3. As previously reported by others2,4,5,6, there was a significant increase in IgG reactivity to RBD between priming and boosting (P<0.0001) (Fig. 1a). IgM and IgA titers were lower than IgG titers and remained low after the second vaccine dose (Extended Data Fig. 1a,b).
The magnitude of the response was inversely correlated with age after the bonus (r=−0.54, P=0.005), but in this limited sample the age difference was no longer significant at 1.3 or 5 months after the second dose of vaccine (Extended Data Fig. 1c,d). Between 1.3 and 5 months after the booster, the anti-RBD titers of IgG and IgA decreased significantly. IgG titers decreased on average 4.3-fold (range 1.7-10.2-fold) and loss of activity was directly correlated with time after vaccination (P < 0.0001).